AI System Analyzes Breast Cancer Scans More Accurately than Doctors
One in nine women globally will be diagnosed with breast cancer during their lifetime, and the numbers are only increasing as a result of factors, including increased lifespan and modern lifestyles. Personalized immunotherapy treatment is a necessity now more than ever, but the number of doctors and pathologists who specialize in examining tissue for specific diagnoses needed for personalized medicine is declining. To help combat this problem, Technion researchers have developed an artificial intelligence (AI) neural network that simplifies and improves the diagnostic process. Even better, the network catches potential indicators that are indistinguishable to the human eye, making its assessment more accurate than that of medical personnel.
In order to create the technology, the researchers trained the neural network by showing it 3,376 biopsy scans that either expressed or did not express the PD-L1 protein, which is displayed in some cancerous tumors and acts as a “password” that commands the immune system not to attack the tumor. In cases where PD-L1 presents as a gatekeeper, treating the tumor with specific immunotherapy can convince the body to ignore the password and attack the tumor. The neural network was then tested on biopsy images from 275 patients to indicate whether they were positive or negative for PD-L1, and it achieved 70% accuracy in determining the correct answer. In the remaining 30% of the cases, the network could not make a conclusion based on the visual patterns presented.
Additionally, in situations where the AI disagreed with the pathologist’s initial findings, a second examination showed the AI to be correct – indicating that the variations the AI found were nearly or completely indistinguishable to the human eye, which makes the technology all the more valuable in diagnostics. The neural network can therefore hopefully be used to assist doctors in making or verifying a diagnosis, matching the best treatment to the individual patient, and offering a prognosis.
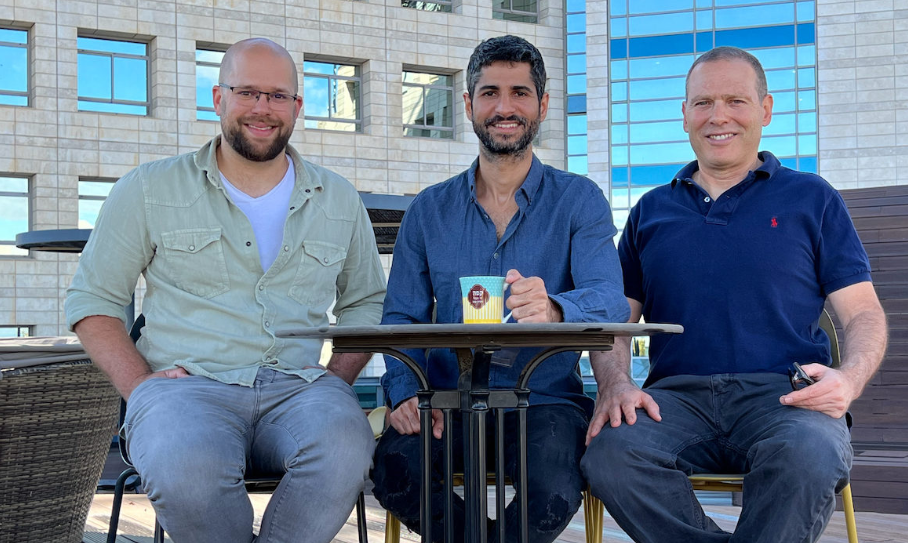
The team’s findings were recently published in Nature Communications. The researchers included Professors Gil Shamai, Amir Livne, and Ron Kimmel from the Henry and Marilyn Taub Faculty of Computer Science and Clinical Assistant Professor Gil Bar-Sela from the Ruth and Bruce Rappaport Faculty of Medicine, along with others hailing from the Institute of Molecular Pathology and Immunology of the University of Porto (Ipatimup) in Portugal and Carmel Medical Center in Haifa, Israel.
Technion Students Lauded for Novel Method for Decreasing Hair Loss from Chemotherapy

Recently, a team of 12 Technion undergraduates competed in the prestigious iGEM competition in Paris, France. Led by Maia Lehrman, they presented their research for developing a way to reduce hair loss in chemotherapy patients by using a bacteria called decursin.
Decursin is derived from a plant, Angelica gigas – grown exclusively in China and Korea – that has the ability to prevent apoptosis, or programmed cell death, including in hair cells. The project focused on engineering bacteria enzymes to create more decursin bacteria, since the plant is very rare and only contains a small amount of decursin. Their ultimate goal is to develop a scalable method for producing decursin and then adding it to shampoos, creams, and other products to reduce hair loss for chemotherapy patients.
According to Lehrman, the idea for the project came from speaking with teammate Baraah Rashed’s neighbor, who was battling cancer and receiving chemotherapy treatments. Through speaking with her, the team learned of the distress the neighbor was going through as a result of losing her hair, which led to the team researching induced hair loss and ways to prevent it. The team hopes to continue their research using the method that earned them a first-place win for having the most precise biological measurement methods and which was led by team members Iser Snoyman and Mattan Hoory.
The team was also recognized as the best bio-manufacturing project. Additionally, they were ranked in the top four teams in six other categories, including one for giving the best presentation.
The prestigious iGEM Competition was initiated by the Massachusetts Institute of Technology in 2004 to give students an opportunity to experiment in synthetic biology. Technion teams have been competing in iGEM and winning since 2012 under Professor Roee Amit, head of the Synthetic Biology Laboratory for the Decipherment of Genomic Codes.
This year’s group was comprised of students from a variety of faculties including biomedical engineering, computer science, biotechnology, food engineering, and more. The team members were Team Captain Maia Lehrman, Nova Noiman, Baraah Rashed, Mattan Hoory, Yasmin Habib, Iser Snoyman, Mazal Faraj, Amit Nelkin, Irina Shkalikov, Yana Shklovski, Reut Laufer, and Ran Benayoun.
Technion Scientists Propose Revolutionary New Framework for Cancer Research

In a revolutionary new discovery, Technion researchers Aseel Shomar, Professor Omri Barak, and Professor Naama Brenner propose that cancer cells are able to learn and adapt to changing environments in order to survive. Equipped with this knowledge, researchers are now investigating better ways of treating — and perhaps curing — cancer.
It is commonly thought that both drug resistance and the ability to metastasize appear in cancer cells as random mutations. Since such a mutation is advantageous to cancer cells, enabling them to survive in an environment that attempts to fight them, these mutations become dominant. However, mounting evidence from research groups around the world do not seem to match this hypothesis, and treatment plans based on this theory do not significantly increase patients’ life expectancy. Now, Aseel Shomar, Prof. Barak, and Prof. Brenner propose a new hypothesis that matches the evidence at hand: cancer cells learn and adapt to their environment, enabling them to develop drug resistances and conform to the new environments of metastasis locations.
While cancer cells have no brain, they are sensitive to stress, and seek ways of reducing stress through a trial-and-error process within their gene regulatory network. An interaction that reduces stress gets strengthened.
While tumors that learn and adapt might sound like a nightmare, Ms. Shomar, Prof. Barak, and Prof. Brenner also found reason for hope. The same mutations found to promote cancer in our body can be carried by cells that remain healthy. Even cells from active tumors, transported into healthy tissue, were in some experiments “cured,” reverting to their non-cancerous state.
“There is an interaction between the individual cell and the tissue,” Prof. Brenner explains. “The cell has the capacity to explore, but the tissue imposes order and stability. Cancer could perhaps be treated through strengthening the tissue’s ability to calm and control the pre-cancerous cell.” A better understanding of the system, such as the three provide, is a crucial step towards developing more effective treatments.
Most scientific studies add a titbit of data to an existing framework. This is one of a rare category of studies that re-examine existing data and propose a novel framework, offering answers to questions that had hitherto remained unanswered, and opening up new avenues of exploration.
